J.SRINATH REDDY
Roll no. 44
2017 ( 9th semester)
This is an online Elog book to discuss our patient deidentified health data shared after taking his/ her guardians sign informed consent
Here we discuss our individual patient problems through series of inputs from available Global online community of experts with n aim to solve those patient clinical problem with collect6current best evidence based input
This Elog also reflects my patient centered online learning portfolio.
Your valuable inputs on comment box is welcome
I have been given this case to solve in an attempt to understand the topic of " Patient clinical data analysis" to develop my competancy in reading and comprehending clinical data including history, clinical finding, investigations and come up with a diagnosis and treatment plan
CONSENT AND DEIDENTIFICATION :
The patient and the attenders have been adequately informed about this documentation and privacy of the patient is being entirely conserved. No identifiers shall be revealed through out the piece of work whatsoever.
CASE REPORT :
A 50 year old gentleman who is a toddy collector by occupation and resident of Yadadri was brought to the hospital with
CHIEF COMPLAINTS :
* Cough since 3 months
* Fever since 1 month
* Vomitings since 5 days
* Giddiness since 5 days.
HOPI ::
Patient was apparently asymptomatic 3 months ago then he developed cough which was insidious in onset gradually progessing with a quantity of around 2 teaspoon full , foul smelling with yellowish tinge and non blood stained . Then he developed FEVER from 1 month which was insidious in onset with evening rise of temperature , associated with increased sweating and relieves on medication temporarily. Then from the past 5 days he developed VOMITINGS with food as content , non bilious and non foul smelling. He also complained of giddiness for which he was taken to a local hospital and i.v. fluids were given.
Investigations for his cough and fever were done which showed PULMONARY TUBERCULOSIS.
There is also history of loss of weight from 50kgs (3 months ago ) to 35 kgs ( current weight ).
No other adverse history.
PAST HISTORY ::
There was a prior hospital admission 7 years ago due to RIGHT SIDED BACTERIAL PNEUMONIA for which he was treated at a local hospital.
Not a known case of DM , HTN , Asthma , epilepsy .
No history of past blood transfusions or major surgeries.
PERSONAL HISTORY ::
Appetite : decreased since 5 days
Diet : adequate
Sleep : adequate
Bowel and bladder : regular
Addictions : ALCOHOLIC since 30 years
Consumes 90ml of whisky daily.
SMOKER since 30years . Smokes 1 pack ( 20 beedis) per day.
No known drug or food allergies.
FAMILY HISTORY ::
No similar complaints in the family members and also neighborhood.
GENERAL EXAMINATION ::
Patient is conscious , coherent and cooperative , and well oriented to time , place and person.
He is poorly built and weighing 40kgs.
Consent of the patient was taken and examined in a well lighted room.
Pallor - Present
Icterus - absent
Cyanosis - absent
Clubbing - absent
Lymphadenopathy - absent
Edema - absent
VITALS :
Temperature : afebrile
Pulse rate - 78 beats per minute , normal rhythm and character and normal vessel wall , no radio- radial and radio femoral delay.
Respiratory rate - 16 cycles per minute
B.p - 100 / 70 mm of Hg in right arm.

SYSTEMIC EXAMINATION :
RESPIRATORY SYSTEM -
INSPECTION :
Shape- Flattened
Trachea- appears to be central
Apex beat- appears to be near the 5th inter coastal space
Supraclavicular hollow - present both sides
Infraclavicular flattening - present both sides
Suprascapular wasting - present both sides.
Shoulder drooping - absent both sides .
Trail's sign - negative both sides.
Scoliosis/kyphosis/lordosis- absent
No engorged vein sinus or scars seen .


PALPATION :
There is no rise of local temperature or tenderness.
All inspectory findings are confimed.
Trachea- central
Chest movements- Reduced on the right side compared to left side.
Vocal fremitus-reduced on the right side compared to left side.
Rib crowding - absent on both sides
Bony tenderness- absent .
Chest Measurements :
Anteroposterior - 6 inches
Transverse -10.5 inches.
PERCUSSION :
Dullness at mammary and inframammary area on right side .
All other areas are resonant.
Resonance in all areas on left side.
AUSCULTATION :
Right side - breath sounds reduced at mammary and inframammary areas.
Left side - normal
No rhonchi or wheeze heard.
CVS :
S1 , S2 Heard , no murmurs heard
CNS :
No abnormality detected.
PER ABDOMEN :
Soft , non tender , no organomegaly , bowel sounds heard .
CLINICAL DIAGNOSIS :
? RIGHT SIDED TUBERCULAR PNEUMONIA.
INVESTIGATIONS :
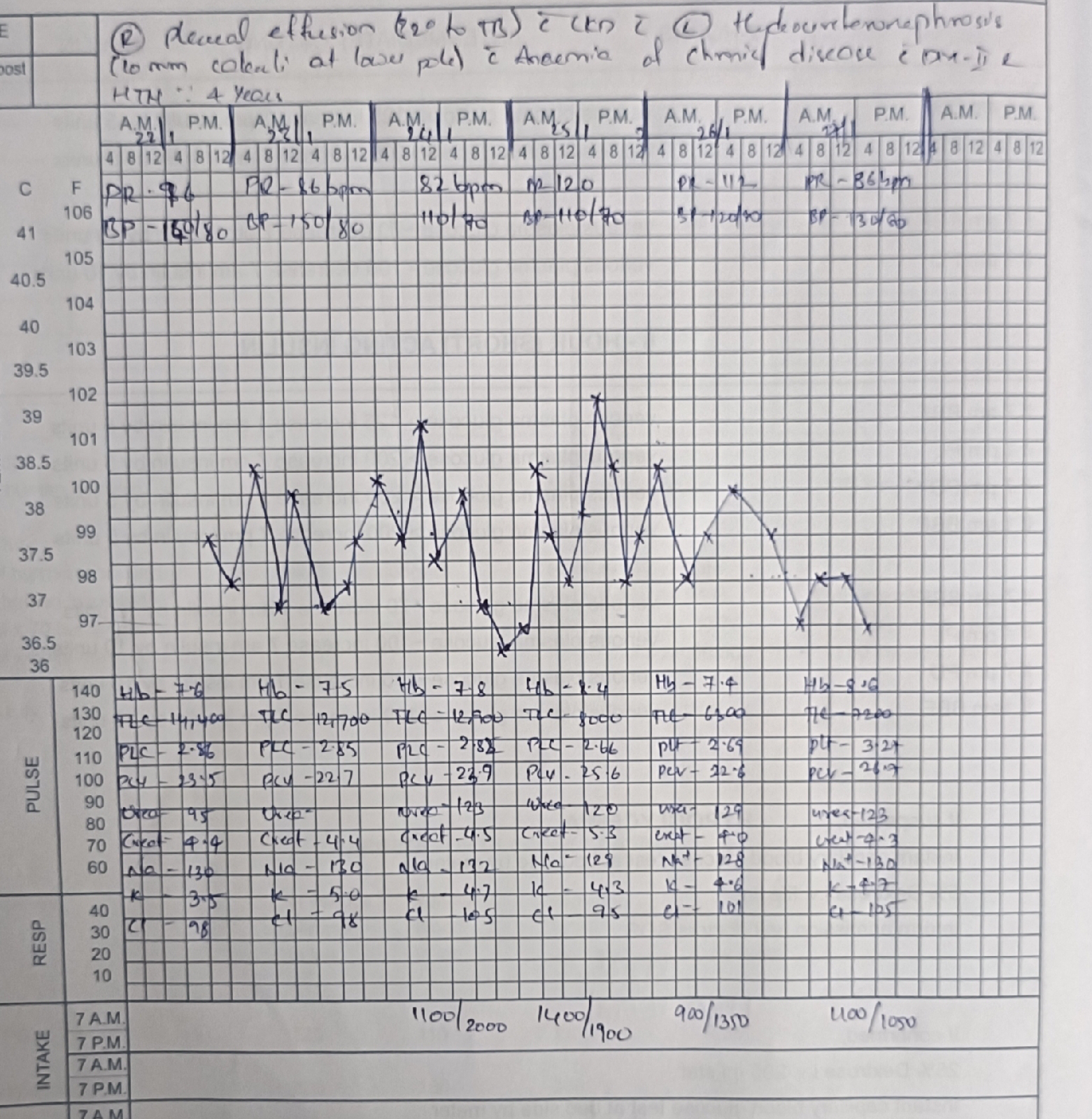
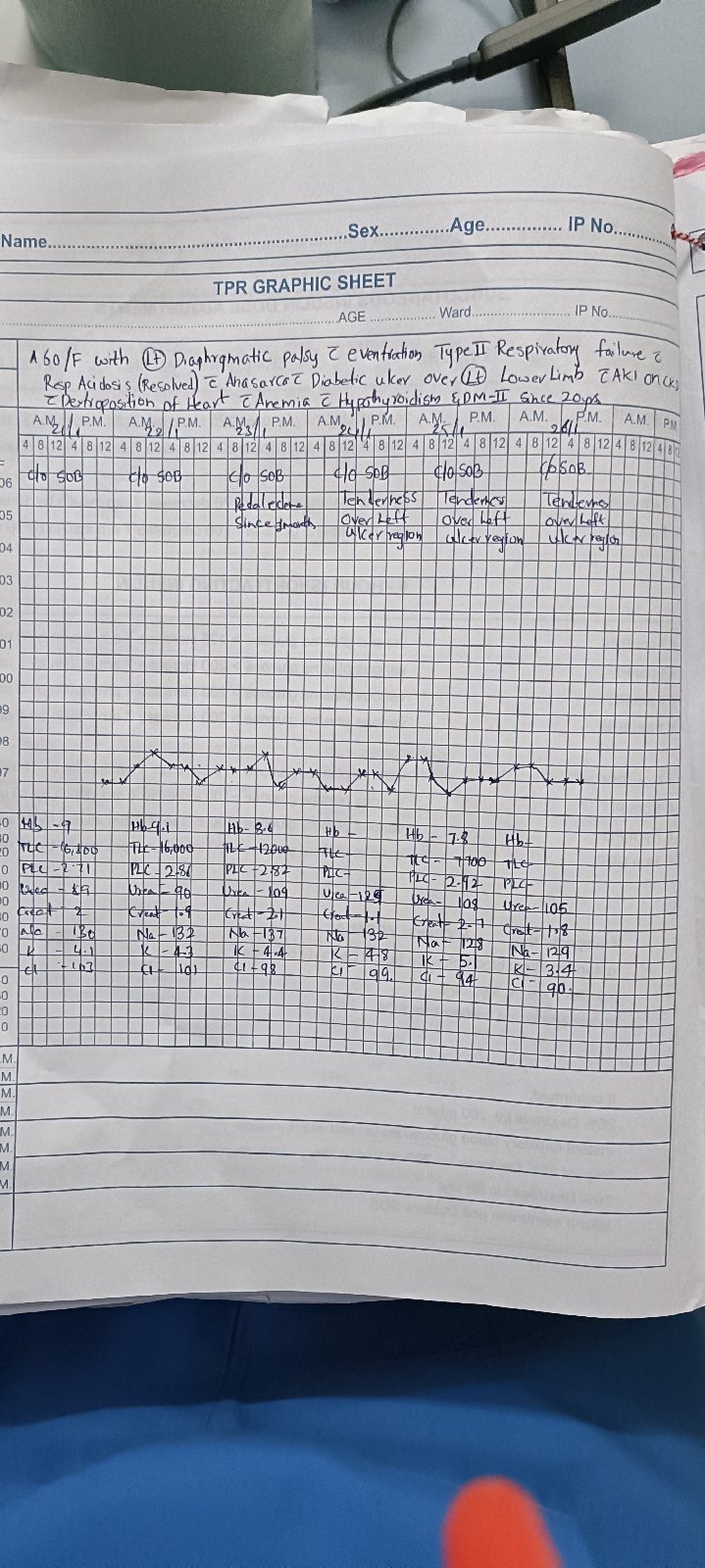
COMPLETE BLOOD COUNTS
Hb 7.58
TLC 9500
Neutrophils 90
Lymphocytes 4
Monocytes 3
Esinophils 3
Platlets 2.51lakhs
Serum blood glucose - 146
Hb1Ac - 6.5
SPUTUM MICROSCOPY
Acid fast bacilli were detected .( Grading - scanty ).

CHEST X - RAY


HRCT of CHEST




LFT ( on day of admission ) :
Total bilirubin 2.83
Direct bilirubin 1.25
AST 230
ALT 175
A/G 1.16
ALP 230
Total proteins 4.2
Albumin 2.26
2D ECHO
EF-55%
Trivial Tr+/no Mr , trivial Ar+
Good LV systolic function +
Diastolic dysfunction +
USG ABDOMEN :
Findings:
1)E/O 5 mm hyperechoic focus noted adherent to Gb wall
Impression :
1) Gall bladder wall edema
2)gall bladder wall polyp
PROVISIONAL DIAGNOSIS :
RIGHT SIDED PULMONARY TUBERCULOSIS. ( confirmed microbilogically )
? Alcoholic hepatitis ( at presentation)
TREATMENT :
1) Ivf ns/ rl @ 100 ml/hr
2)Inj pantop 40 mg IV/od
3)Inj zoefer 4 mg IV/sos
4)tab udilin 500mg po/BD
5)syp potlhlor 10 ml po/tid in glass of water
6)INJ monocef 1gm/IV/BD (day1)
7)2 scoop of protein powder in 100 ml milk/ water po/TID
8)Ascoryl syrup po/TID
9)monitor vitals hourly
10) ATT.
11 ) Thiamine supplementation. Orally




Comments
Post a Comment